- Details
- Category: Health
- Hits: 1858
NEWS
Researchers in New Zealand are conducting two first-of-their-kind randomized controlled trials to assess the usefulness of micronutrients in treating anxiety and depression.
COMMENT
Led by Julia Rucklidge, a Professor of Clinical Psychology at the University of Canterbury in New Zealand, the researchers conducting these trials are hopeful that micronutrients can revolutionize the treatment of anxiety and depression. Certainly, there is already a great deal of scientific evidence that micronutrient-based approaches are helpful in combating such conditions.
In one example of such evidence, a meta-analysis published in 2016 looked at 13 studies involving 1,233 participants and found that supplementation with omega-3 fatty acids can help reduce symptoms of even major depressive disorder.
Other research has found evidence linking a deficiency of B vitamins with depression. A scientific review published in 2017 noted that low levels of B vitamins are common in depression and that supplementation with these nutrients has been shown to improve depression outcomes.
Similarly, a clinical trial published in 2017 showed that magnesium supplements are effective in the treatment of mild-to-moderate depression. Finding that daily supplementation with magnesium leads to a significant decrease in depression and anxiety symptoms, and that it works quickly and is well tolerated, the study concluded that magnesium may be a safe over-the-counter alternative to antidepressant drugs.
Research also suggests eating a vitamin-rich Mediterranean-style diet containing fruit, vegetables, nuts, and fish may help prevent depression.
With close to 10 percent of the world’s population now believed to suffer from depression and/or anxiety, and such disorders said to be costing the global economy one trillion dollars a year, micronutrient and dietary-based approaches could potentially be of enormous benefit to hundreds of millions of mental health patients worldwide.
Read article at nutraingredients.com
Source: https://www.dr-rath-foundation.org/2018/11/micronutrients-for-mental-health-researchers-hopeful-clinical-trials-will-revolutionize-treatment/
- Details
- Category: Health
- Hits: 1780
A new study has found that elderly people who take daily aspirin tablets after a heart attack or stroke are at far greater risk of potentially fatal internal bleeding than originally thought. Published in The Lancet medical journal by scientists at Oxford University, the research suggests that more than 3,000 patients die every year in the UK from long-term use of this drug. Significantly, for people over the age of 75, the risk of suffering a disabling or deadly bleed from aspirin treatment was shown to be ten times higher than for younger patients.
Predictably, rather than recommending safe natural approaches for preventing heart attacks and strokes, the Oxford researchers instead propose the addition of a proton pump inhibitor (PPI), a drug used for reducing gastric acid production, to patients’ medication regimens. They claim that doing so will supposedly cut the risk of bleeding. However, the fact is that PPIs are themselves by no means safe. There is now mounting evidence that long-term use of them increases the risk of cancer, chronic kidney disease, serious allergic reactions, and, ironically, when taken with aspirin, adverse cardiovascular events.
Aspirin depletes body levels of vitamin C
Given that aspirin has long been known to cause fatal bleeding in patients, it is interesting to note that research dating back 80 years shows it depletes body levels of vitamin C. This raises an obvious connection with scurvy, the clinical vitamin C deficiency disease, which similarly results in hemorrhage and death. Seen in this light, the possibility that aspirin fatalities may be related to chronic vitamin C deficiency clearly cannot be discounted.
In a report published in 1936, the first of its type, researchers from the Department of Nutrition at the State University of Iowa in the United States described how administration of aspirin to children was followed by an increased elimination of vitamin C through the urine. Further thought-provoking corroboration came in 1973 in a study published in the Journal of Clinical Pharmacology, which notably found that the presence of aspirin can completely inhibit the uptake of vitamin C into leukocytes (white blood cells).
Aspirin doesn’t prevent diseases, it causes them
The fact that aspirin depletes vitamin C exposes yet again the fraudulent strategy of the pharmaceutical business with disease; namely, to design and promote
synthetic chemical drugs that cause, as opposed to prevent or cure, diseases. Employed for more than a century now, the use of this unethical tactic for increasing drug markets has enabled the pharma industry to achieve global sales of over one trillion dollars a year. Another example can be seen in calcium channel blockers, a frequently prescribed class of cardiovascular medication. A study conducted at the Dr. Rath Research Institute published in 2016 proved that these too obstruct the uptake of vitamin C by cells. This explains the reason behind the increased risk of heart disease, breast cancer, and gum problems reported in many clinical studies using these drugs.
In a similar way, while aspirin is claimed to prevent heart attacks and strokes, the reality is that by depleting vitamin C it actually contributes to these outcomes. For as Dr. Rath’s scientific discovery and research conducted at the Dr. Rath Research Institute has shown, cardiovascular disease is a direct result of chronic vitamin C deficiency and is essentially an early form of scurvy.
The original patent on aspirin was held by the German drug and chemical company Bayer, a former member of the IG Farben Cartel, who first marketed the chemical in 1899. Despite the existence of studies proving that it depletes vitamin C, to this day Bayer continues to promote aspirin as reducing the risk of heart attacks and strokes and openly portrays it as a “wonder drug.”
There’s an old saying that there’s no such thing as a safe drug. As the facts about aspirin remind us, this observation remains as true today as it ever was.
- Details
- Category: Health
- Hits: 2208
The Movement of Life Cyprus has organized a lecture with Dr. Matthia Rath, a German researcher on the topic:
Innovative and scientifically-established discoveries on natural approach of cardiovascular disease.
University of Nicosia 27 03 2018
- Details
- Category: Health
- Hits: 1787
Frequently prescribed drugs that treat cardiovascular conditions may lead to weakening of the blood vessel walls.
Drugs intended to reduce blood pressure, as well as correct arrhythmias and some forms of heart disease, are the most commonly prescribed pharmaceuticals in the United States (US) today. One in every three adults, or approximately 75 million people, is diagnosed with high blood pressure in the US and many more have pre-hypertension. Around 15 million patients in the US have some form of irregular heartbeats, or arrhythmias. The most commonly prescribed drugs to treat these and other conditions are the so-called “channel-blockers” or “agonists”, which include calcium, sodium and potassium channel blockers. Sales of these drugs have reached $6 billion worldwide. In the US, calcium channel blockers are the eighth largest drug class by prescription sales.
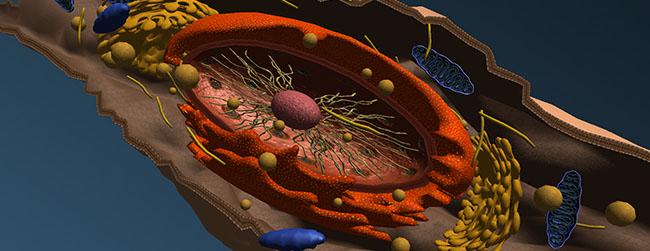
These drugs prevent calcium (and other valuable minerals) from entering the inside of the cells by blocking specific channels located in the walls of the smooth muscle cells lining the blood vessels, the cardiac muscle cells (myocytes), and other tissues. By blocking these channels, the drugs cause relaxation of the cells and other pharmacological effects. Sodium transport channels are also used by Vitamin C to enter the cells.
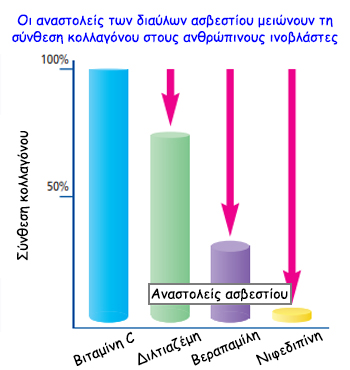
A new study conducted at the Dr. Rath Research Institute and published in the American Journal of Cardiovascular Disease¹ shows that, in addition to blocking the entry of calcium, these drugs obstruct the uptake of vitamin C by the cells. Vitamin C is an essential nutrient for the production of collagen – the key stability molecule for blood vessel walls and connective tissue in general. Its long-term deficiency is especially detrimental for the cells building the artery walls as it can cause microscopic structural damage, followed by the build-up of atherosclerotic deposits – the cause of heart attacks and strokes. The study indicates that among the studied channel blockers, nifedipine (i.e., Procardia, Nifediac) has the most pronounced effect, causing a significant decrease of collagen production by the human vascular muscle cells. Taking into account that these drugs are supposed to be used for an indefinite time, their detrimental health consequences are of great concern.
In this aspect, the study shows that calcium-blocker-induced inhibition of collagen production by the cells can be compensated for by providing vitamin C. In particular, supplying fat-soluble vitamin C (ascorbyl palmitate), rather than simple vitamin C, resulted in significantly higher vitamin C concentration within the cells, further supporting collagen production.
The fact that calcium channel blockers – taken by tens of millions of heart patients worldwide in the belief that they can help prevent heart attacks – are actually increasing the risk for heart attacks due to weakening of the heart muscle and blood vessel walls, has been a major impediment in cardiology. In addition, increased risk of breast cancer and gum disease has also been reported. Based on the new study results it is possible that many of the side effects of these medicines could be prevented simply by supplementation of a synergistic combination of vitamin C, including ascorbyl palmitate, and other essential micronutrients.
Reference Ivanov V, et al., Am J Cardiovasc Dis 2016:6(2):26-35
Source: Dr. Rath Health Foundation
Page 4 of 4