Frequently prescribed drugs that treat cardiovascular conditions may lead to weakening of the blood vessel walls.
Drugs intended to reduce blood pressure, as well as correct arrhythmias and some forms of heart disease, are the most commonly prescribed pharmaceuticals in the United States (US) today. One in every three adults, or approximately 75 million people, is diagnosed with high blood pressure in the US and many more have pre-hypertension. Around 15 million patients in the US have some form of irregular heartbeats, or arrhythmias. The most commonly prescribed drugs to treat these and other conditions are the so-called “channel-blockers” or “agonists”, which include calcium, sodium and potassium channel blockers. Sales of these drugs have reached $6 billion worldwide. In the US, calcium channel blockers are the eighth largest drug class by prescription sales.
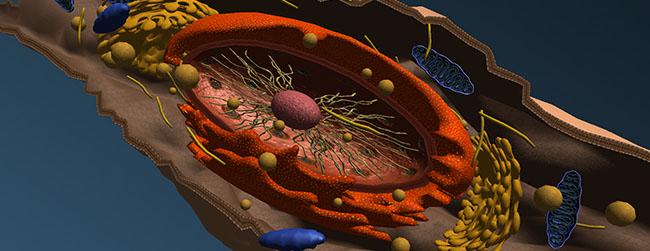
These drugs prevent calcium (and other valuable minerals) from entering the inside of the cells by blocking specific channels located in the walls of the smooth muscle cells lining the blood vessels, the cardiac muscle cells (myocytes), and other tissues. By blocking these channels, the drugs cause relaxation of the cells and other pharmacological effects. Sodium transport channels are also used by Vitamin C to enter the cells.
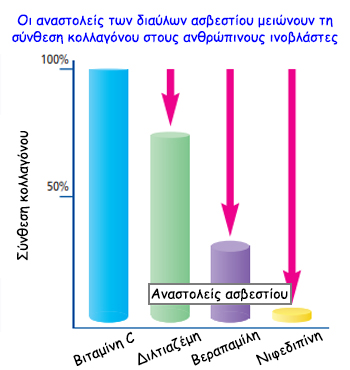
A new study conducted at the Dr. Rath Research Institute and published in the American Journal of Cardiovascular Disease¹ shows that, in addition to blocking the entry of calcium, these drugs obstruct the uptake of vitamin C by the cells. Vitamin C is an essential nutrient for the production of collagen – the key stability molecule for blood vessel walls and connective tissue in general. Its long-term deficiency is especially detrimental for the cells building the artery walls as it can cause microscopic structural damage, followed by the build-up of atherosclerotic deposits – the cause of heart attacks and strokes. The study indicates that among the studied channel blockers, nifedipine (i.e., Procardia, Nifediac) has the most pronounced effect, causing a significant decrease of collagen production by the human vascular muscle cells. Taking into account that these drugs are supposed to be used for an indefinite time, their detrimental health consequences are of great concern.
In this aspect, the study shows that calcium-blocker-induced inhibition of collagen production by the cells can be compensated for by providing vitamin C. In particular, supplying fat-soluble vitamin C (ascorbyl palmitate), rather than simple vitamin C, resulted in significantly higher vitamin C concentration within the cells, further supporting collagen production.
The fact that calcium channel blockers – taken by tens of millions of heart patients worldwide in the belief that they can help prevent heart attacks – are actually increasing the risk for heart attacks due to weakening of the heart muscle and blood vessel walls, has been a major impediment in cardiology. In addition, increased risk of breast cancer and gum disease has also been reported. Based on the new study results it is possible that many of the side effects of these medicines could be prevented simply by supplementation of a synergistic combination of vitamin C, including ascorbyl palmitate, and other essential micronutrients.
Reference Ivanov V, et al., Am J Cardiovasc Dis 2016:6(2):26-35
Source: Dr. Rath Health Foundation